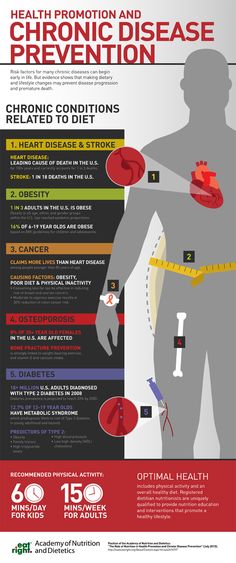
Chronic diseases are long-term medical conditions that are often progressive and require ongoing care. Common examples include heart disease, diabetes, cancer, arthritis, and chronic respiratory conditions. Managing chronic diseases involves more than just addressing symptoms—it requires a comprehensive approach that incorporates medical treatment, lifestyle changes, and continuous monitoring.
Here's what you need to know about treating chronic diseases:
Understanding Chronic Diseases
Chronic diseases differ from acute conditions in that they persist over time and often cannot be cured, but they can be managed effectively. The goal of chronic disease treatment is to control symptoms, improve quality of life, and prevent complications or worsening of the condition. Treatment strategies vary depending on the specific disease, but the principles of chronic disease management often share common elements.
Medical Management
Medication: Medications are a cornerstone of chronic disease treatment. Depending on the condition, medications may be prescribed to control symptoms, slow disease progression, or manage complications. For example:
Diabetes: Insulin or oral medications help control blood sugar levels.
Heart disease: Medications such as statins, beta-blockers, and blood thinners may be used to manage cholesterol levels, blood pressure, and heart function.
Arthritis: Anti-inflammatory drugs or disease-modifying antirheumatic drugs (DMARDs) may be prescribed to reduce pain and inflammation.
Regular monitoring by a healthcare provider is essential to ensure the effectiveness of medications and to make adjustments as needed.
Surgery and Interventions: In some cases, surgical interventions may be required. For instance, heart disease patients might need procedures such as angioplasty or bypass surgery, while patients with chronic kidney disease might require dialysis or a kidney transplant.
Rehabilitation Therapies: Physical therapy, occupational therapy, and speech therapy can play significant roles in treating chronic diseases. For example, people with arthritis may benefit from physical therapy to improve joint function, while patients recovering from strokes may need rehabilitation to regain motor skills.
Lifestyle Modifications
Diet and Nutrition: Diet plays a critical role in managing many chronic diseases. Patients with diabetes, for example, must monitor carbohydrate intake, while those with heart disease should focus on reducing saturated fat, cholesterol, and sodium. Working with a nutritionist can help create a diet plan tailored to the specific needs of the disease.
Exercise: Regular physical activity is crucial for managing chronic diseases such as obesity, heart disease, and diabetes. Exercise helps to improve cardiovascular health, regulate blood sugar levels, reduce inflammation, and maintain joint mobility. It’s important to follow a personalized exercise plan based on the patient’s condition and physical capabilities.
Weight Management: Maintaining a healthy weight can reduce the risk of complications from chronic diseases like diabetes, heart disease, and hypertension. Weight loss through a combination of diet and exercise can significantly improve health outcomes for patients with obesity-related chronic conditions.
Smoking Cessation: Smoking is a major risk factor for many chronic diseases, including heart disease, chronic obstructive pulmonary disease (COPD), and cancer. Quitting smoking is essential to improving lung function, reducing the risk of complications, and enhancing overall health.
Stress Management: Chronic stress can worsen many chronic diseases, particularly those related to heart health and immune function. Mindfulness practices, relaxation techniques, counseling, and social support can help patients manage stress more effectively.
Regular Monitoring and Follow-Up
Routine Check-Ups: Regular check-ups with healthcare providers are essential for managing chronic diseases. These appointments allow for the monitoring of symptoms, adjustment of medications, and early detection of potential complications.
Self-Monitoring: Many chronic diseases require patients to actively monitor their health. For example, individuals with diabetes need to regularly check their blood sugar levels, while those with hypertension should monitor their blood pressure at home. Self-monitoring empowers patients to stay in control of their health.
Screening for Complications: Chronic diseases often increase the risk of other health complications. Patients should undergo regular screening for associated issues. For example, diabetes patients should have their eyes, kidneys, and feet checked regularly to prevent complications like retinopathy, nephropathy, and neuropathy.
Adherence to Treatment Plans: Following the prescribed treatment plan is crucial for managing chronic diseases effectively. Patients who adhere to their medication regimens, attend medical appointments, and maintain recommended lifestyle changes are more likely to experience positive health outcomes.
Support Systems
Healthcare Team: Chronic disease management often requires a multidisciplinary approach. This may include primary care physicians, specialists, nurses, dietitians, physical therapists, and mental health professionals. Working closely with a healthcare team ensures that all aspects of the disease are being addressed.
Patient Education: Educating patients about their condition is key to effective management. Patients should understand the nature of their disease, how to manage symptoms, and how to recognize warning signs of complications. This empowers them to take an active role in their care.
Family and Social Support: Emotional and practical support from family and friends can make a significant difference in a patient’s ability to manage their chronic condition. Support groups, whether in-person or online, can also provide encouragement, advice, and shared experiences from others facing similar challenges.
Psychological and Emotional Well-Being
Living with a chronic disease can take a toll on mental health, leading to feelings of anxiety, depression, or frustration. Psychological support, including counseling or therapy, can be essential in helping patients cope with the emotional burden of chronic illness. Integrating mental health care into chronic disease management can improve overall well-being and health outcomes.